Building Resilience Through Trauma-Informed Care
Shifting the perspective from “what’s wrong with you?” to “what happened to you?”
By Lucy Preysz, Communications & Policy Coordinator
According to data from the National Survey of Children’s Health on adverse childhood experiences, almost half of all of the nation's youth aged 17 and under have experienced at least one serious childhood trauma, which equates to nearly 35 million children.
Additionally, the landmark Adverse Childhood Experiences (ACE) study, documented that there is a strong relationship between exposure to adverse childhood experiences and risk of long-term health risks.
In order to address childhood trauma and adversity and build resilience, we must shift our perspective from “What’s wrong with this child?” to “What happened to this child?” In order to shift this perspective, we first need to build awareness in our community that trauma is very common.
What is “Trauma-Informed Care (TIC)”?
With trauma-informed care, we start with an understanding that any person may have experienced some degree of trauma, and that it’s supportive to work with people in ways that build resilience and prevent the possibility of re-traumatization.
Trauma-Informed Care Implementation Resource Center explains TIC:
A trauma-informed approach to care acknowledges that health care organizations and care teams need to have a complete picture of a patient’s life situation — past and present — in order to provide effective health care services with a healing orientation.
This approach doesn’t solely rely on mental health professionals, as Child Trends states:
TIC is not the sole responsibility or purview of mental health professionals. While evidence-based trauma treatment can play a significant role in the healing process for children who need it, there are many other ways to implement TIC. In fact, every program and service system that touches the lives of children can play an important role.
In order to build resilience among children and youth, we must implement TIC into our child and family services system through our roles as parents, educators, clinicians, organizational leaders, service providers, families and policy makers.
What Does Trauma Look Like?
Clare Norelle is a certified facilitator of Trauma Center Trauma-Sensitive Yoga (TCTSY) and the Community Resiliency Model (CRM), who offers individual sessions through Dane County’s Comprehensive Community Services (CCS) program. Clare explains how trauma affects many aspects of a person’s life, and presents itself in a variety of different forms:
You can develop trauma from experiences of neglect, abuse, violence, loss, illness, injury, marginalization, or oppression—or other experiences that feel overwhelmingly harmful. Sometimes trauma can happen from witnessing or being in close contact with the trauma of other people. Sometimes it happens all at once, and sometimes it’s more cumulative, with traumatic stress increasing over time.
Trauma is a condition that mainly affects your autonomic nervous system. It can make you feel wound up, anxious, angry or hyper-vigilant, with difficulty sleeping… or shut down, numb, depressed or sluggish, with a hard time feeling alert…. Or a strange combination of these and other things. Trauma can affect your moods, your memory, your appetite, your sense of time, and how or whether you’re able to see and hear things. It can diminish your ability to accurately feel what’s going on in your body in the present moment, to process information and make decisions, and to stay present and attentive in your life. Trauma can compromise your immune system and your overall health, and it can have a major impact on your life.
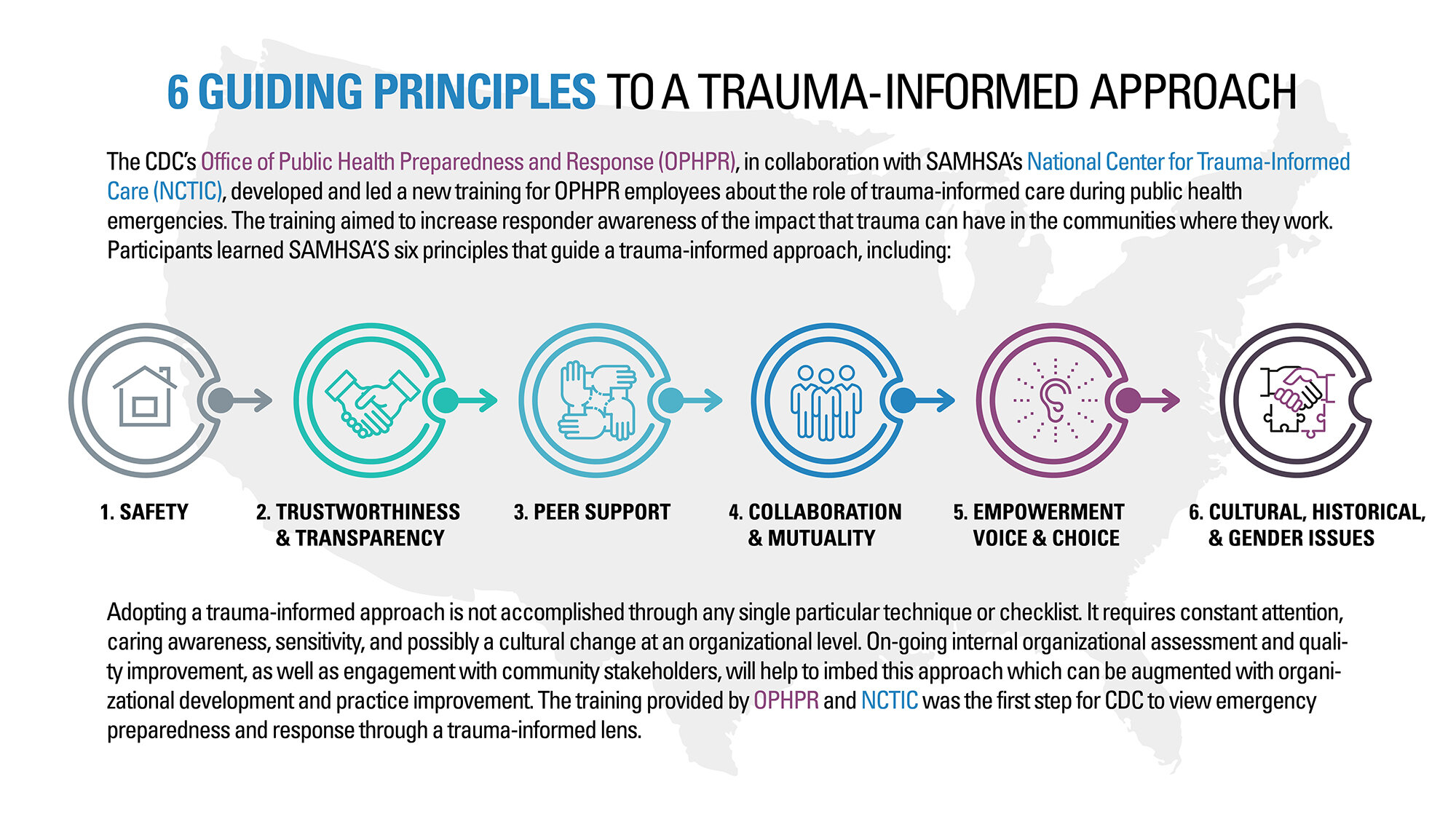
Key Components of a Trauma-Informed Approach
The six principles, as described in the infographic, that guide a trauma-informed approach include:
Safety
Trustworthiness & transparency
Peer support
Collaboration & mutuality
Empowerment & choice
Cultural, historical & gender issues
For additional guidance on implementing a trauma-informed approach, additional information can be found here.
What is resilience?
According to the Administration for Children and Families, resilience is defined as “the ability of individuals to not succumb to adverse experiences and is the typical response to adversity”.
It’s important to note that trauma can sometimes create negative coping mechanisms, such as substance abuse, which can make it challenging, but not impossible, to build resilience.
Trauma itself doesn’t make someone less resilient; resilience can be learned and developed over time with learning proper resilience-building skills, such as developing positive coping strategies and habits.
Community Resilience Model (CRM)®
The primary focus of this skills-based, stabilization program is to reset the natural balance of the nervous system. CRM’s goal is to help to create “trauma-informed” and “resiliency-focused” communities that share a common understanding of the impact of trauma and chronic stress on the nervous system and how resiliency can be restored or increased using this skills-based approach.
The following information can be found in Clare Norelle’s article, “Trauma and Healing in the Body” on her website:
The six practices of CRM are meant to be accessible, easily practiced, and easily shared with people of all ages. They also work to deepen connection and integration in the nervous system:
Tracking sensations: learning to feel and distinguish sensations of well-being (resilient zone), activation (high zone) and shut-down (low zone) created in your autonomic nervous system. These zones correspond well with Stephen Porges’ descriptions of the ventral vagal or social engagement response (resilient zone); the sympathetic nervous system response (high zone), and the dorsal vagal response (low zone).
Resourcing: helping your body return to its resilient zone by recalling memories, visualizations, and other things which for you promote a sense of calm.
Grounding: bringing your attention to the places where your body is in contact with ground, or with some other form of support that feels steadying for you (feet on the ground; hands pushing against a wall; seat in a chair).
Gesturing: exploring movements which for you embody feelings of joy, peacefulness, love, and other emotions that tend to strengthen resilience.
Shift and Stay: using the skills of resourcing, grounding, or gesturing to center your nervous system in its resilient zone, then tracking what you feel as you stay there for a while. This strengthens neural connectivity to sensations of well-being, which allows you to more easily return to those sensations.
Help Now: a set of ten simple strategies that can help bring you back into your resilient zone, when practiced with attentiveness to sensations: going for a walk; pushing against a wall; looking attentively at something; counting; drinking water; touching an object, feeling temperature, listening for sounds, touching something in nature, and noticing what you notice in the world around you.
To learn more about Clare Norelle’s work, including free online yoga classes, CRM trainings, trauma healing resources, and other information, you can visit: clarenorelle.com